Cultures and communities who’ve practiced fasting for years know the health benefits well through their own lived experience. But research is starting to catch up, and we’re seeing countless studies being published that point to the many positive health outcomes associated with fasting.
Intermittent fasting in particular has become quite popular and more mainstream in recent years, and the bulk of fasting research tends to be on this method. However, there’s a vast and growing body of research on different approaches to fasting, showing that it may:
- reverse insulin resistance
- modulate the inflammatory response
- stimulate autophagy (clearing cellular debris)
- promote DNA repair
- reduce oxidative stress
- normalize cholesterol
- reduce body weight / fat mass
- reduce the risk of diabetes, cardiovascular disease, cancers, and neurologic disorders
While some might see fasting as a health fad or weight loss trend, there’s substantial science-backed evidence on the benefits of fasting for health and longevity.¹ The real impact is much deeper than what we’re able to observe on the surface; fasting can be a powerfully transformative tool when practiced correctly.
Our previous post explored the impact of fasting on insulin resistance. In this article, we’ll dive a bit deeper into the ways that fasting can promote immune health and reduce inflammation in the body.
In a recent study conducted by Mount Sinai Health Systems and published by Cell, researchers found that “fasting improves chronic inflammatory diseases without compromising monocyte emergency mobilization during acute infectious inflammation and tissue repair. These results reveal that caloric intake and liver energy sensors dictate the blood and tissue immune tone and link dietary habits to inflammatory disease outcome.”²
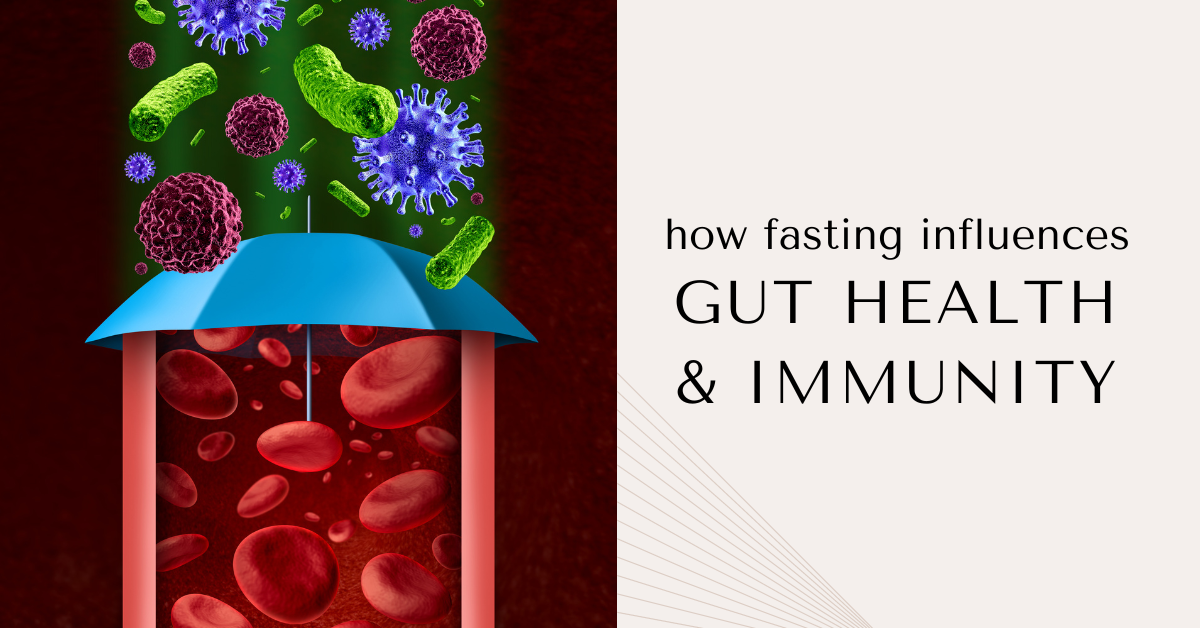
What’s the gut got to do with it?
The body’s immune response is closely connected to the gut microbiome with a bidirectional relationship. In fact, about 70% of the body’s immune system is located in the gut, and these cells play a significant role in systemic immunity.
The gut microbiome is the collection of trillions of bacteria that live in your gut and influence many physiological functions. More than just supporting digestion, these bacteria also impact immunity, cognitive function, mood, sleep, weight and cardiovascular health. The diverse microbiome begins developing while we’re in the womb and is shaped by many factors, some of which we can’t control (like genetics, trauma or illness), and others that we’re able to influence with healthy nutrition and lifestyle practices.
When everything is functioning normally, the gut supports the immune system by modulating healthy immune responses, while the immune system helps to populate the gut with healthy bacteria. Cells in the gut produce proteins called cytokines, which regulate various inflammatory responses and act as messengers between cells.
Cytokines are important moderators in maintaining intestinal homeostasis by governing key cellular processes and responses to disease and infection. However, gut dysbiosis (an imbalance of bacteria in the gut) is often linked to immune responses that cause abnormal production of these inflammatory cytokines.
 Some of the symptoms people experience with gut dysbiosis include:
Some of the symptoms people experience with gut dysbiosis include:
- digestive disorders
- chronic fatigue
- brain fog
- anxiety and depression
- heartburn and acid reflux
- abdominal discomfort
- food sensitivities, gas and bloating
- aching joints
- headaches
- sinus issues
- acne and other skin conditions
These changes in the microbiome can lead to chronic inflammation and metabolic dysfunction, including type 2 diabetes, stroke and obesity-related illness. Gut dysbiosis is also a leading cause of leaky gut syndrome, and numerous studies have shown links between gut health and endocrine disorders, cardiovascular disease, cancer, mental health, and of course, the immune system.
So, it’s clear that the health of the gut and the immune response is closely connected and is largely influenced by our dietary choices. Eating a diet high in processed foods, refined carbs, added sugars, alcohol and unhealthy fats disrupts the gut microbiome and can lead to systemic inflammation. Reducing or eliminating these things from your diet and choosing foods that support gut health will help you to repopulate the healthy bacteria and restore balance.
Fasting, gut health and immunity
Fasting takes healing in the gut a step further. When we remove the foods that contribute to gut dysbiosis and give the digestive system a rest, we’re starving the bad bacteria that’s causing inflammation and altering the immune system. However, the foods we choose to refuel with in an eating window are equally influential (or maybe even more-so) in this process; your refeed following a fast is an important opportunity to choose the right nutrients and probiotics to restore a healthy microbiome.
Fasting also signals the process of autophagy – the physiological mechanism of clearing debris and damaged cells to encourage cellular repair – after a period of about 2-4 days. The body has incredible regenerative ability when it receives the right messages. Fasting upregulates autophagy, more effectively clearing toxins and waste that may otherwise lead to chronic inflammation and disease.
Upgrade your metabolic health
We begin a new session of our very popular Metabolic Upgrade program TOMORROW! This is an opportunity to deepen the connection to our bodies and ourselves, as well as to examine our relationships with food, activity, thought processes and patterns, and the people in our lives.
If you’d like to learn more about fasting and how to prepare yourself for a healthy fast, sign up for our 4-week online Metabolic Upgrade program and start making small changes that can lead to major transformation.
Sources:
- https://blog.insidetracker.com/intermittent-fasting-impacts-longevity-summary-research#:~:text=During%20fasting%2C%20cells%20undergo%20an,including%20diabetes%20and%20cardiovascular%20disease.
- https://www.cell.com/cell/fulltext/S0092-8674(19)30850-5
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7474734/
- https://www.ifm.org/news-insights/gut-health-immune-response/
- https://www.clevelandclinicabudhabi.ae/en/health-byte/pages/fasting-health-immunity-is-there-a-connection.aspx
- https://nutrition.bmj.com/content/early/2022/06/30/bmjnph-2022-000462
- https://www.frontiersin.org/articles/10.3389/fnut.2022.871682/full